4 Minutes
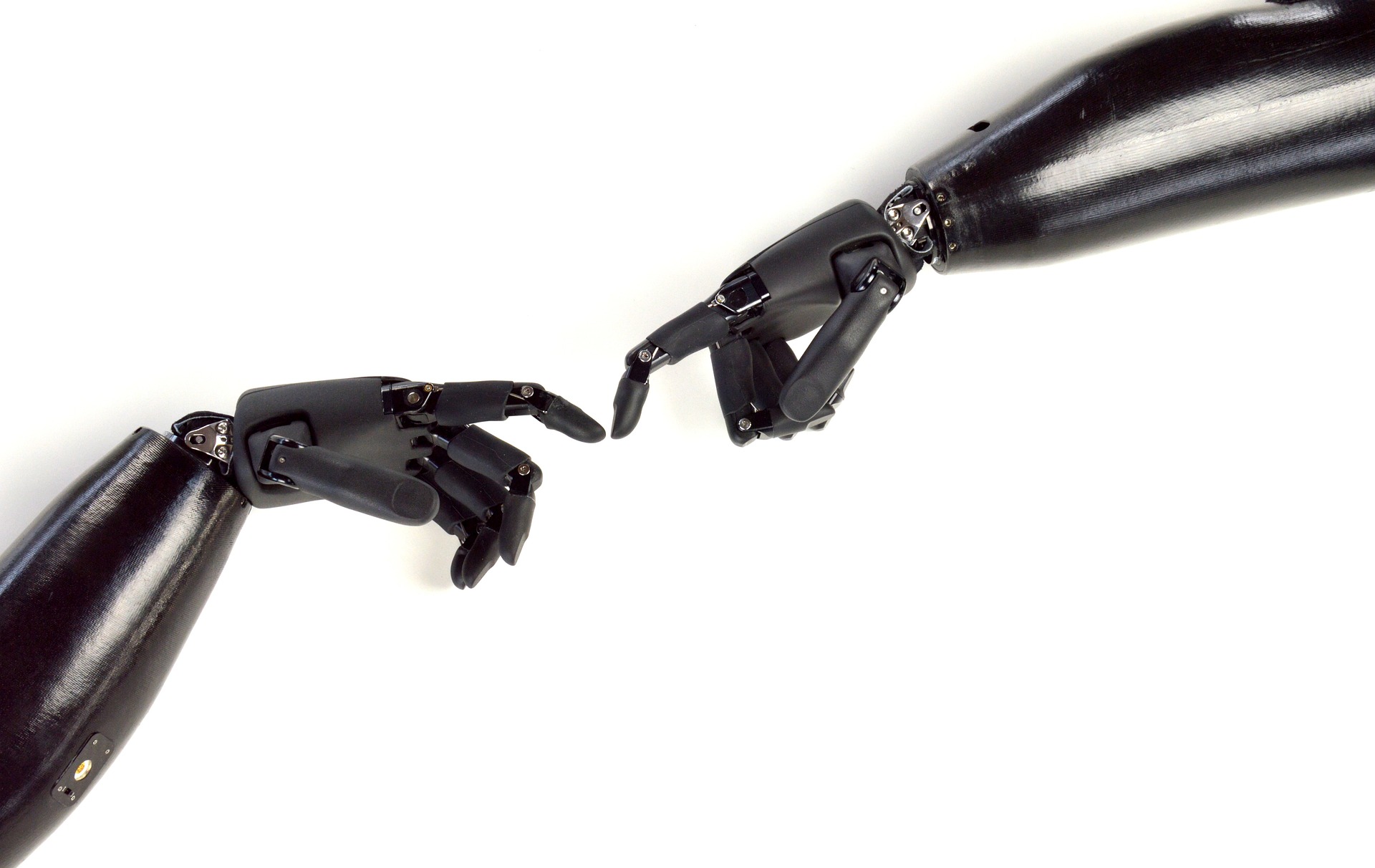
Biomaterials in Regenerative Medicine: A Look at Current Innovations and Future Directions
Biomaterials are essential in regenerative medicine, offering promising solutions for repairing and regenerating damaged tissues and organs. These materials provide scaffolding that supports cell growth, guides tissue development, and integrates with the body. The...
Read More